What is Pulmonary Hemorrhage?
Pulmonary hemorrhage can be described as the bleeding that occurs at the level of the lungs, with more than just one cause possible. There are two main categories, meaning the diffuse pulmonary hemorrhage (variant – diffuse alveolar hemorrhage) and the localized pulmonary hemorrhage.
The acute bleeding can extend to the upper respiratory tract, affecting the trachea. If the patient presents clinical signs, it is suggestive of a massive hemorrhage taking place. Blood can ooze either from the nose or the mouth (to a lesser extent, from other places as well). The patient’s breathing becomes rapidly worse and the patient can suffer from progressive cyanosis, followed by vascular shock.
Pulmonary Hemorrhage in Newborns and Small Infants
The prognosis of the pulmonary hemorrhage is determined by the underlying cause that has led to such problems in the first place. This condition affects newborns and especially those who have been born before the due term. The incidence of the pulmonary hemorrhage is of 1 in every 1000 live births. Unfortunately, the rate of mortality is quite high (30-40%).
In newborns and small infants, these are the most common causes that lead to the appearance of the pulmonary hemorrhage (predispose to perinatal asphyxia and/or hemorrhage):
- Infant prematurity (most common association)
- Toxemia of pregnancy
- Maternal cocaine use
- Erythroblastosis fetalis
- Breech delivery
- Hypothermia
- Infant respiratory distress syndrome
- Administration of exogenous surfactants
- Extracorporeal membrane oxygenation.
The symptoms that newborns experience are mainly due to the hemorrhagic pulmonary edema. Laboratory studies performed on these patients show a hematocrit that is lower than normal (with 15-20% less than it should be). Moreover, the concentration of the small proteins is high, in comparison to the plasma levels.
The asphyxia associated with problematic births places serious pressure on the heart, with a high risk for heart infarction; because of such changes, the pulmonary microvascular pressure increases and the pulmonary hemorrhage occurs (edema). There are a number of factors that are associated with such changes, meaning: plasma proteins in low concentration, damage to the lungs, hypovolemia and high alveolar surface tension. These factors are known to favor the increased filtration at the level of the pulmonary capillaries.
Diffuse Pulmonary Hemorrhage
The diffuse pulmonary hemorrhage refers to a particular type of hemorrhage where the bleeding at the level of the lungs is diffuse. If the bleeding occurs at the level of the alveolar spaces, then the hemorrhage can be presented as the diffuse alveolar hemorrhage. This form of hemorrhage is most common in young people, aged between 18 and 35 years. Another form is represented by the idiopathic pulmonary hemosiderosis – this is generally diagnosed in children who are under 10 years of age. The main cause is believed to be a defect at the level of the alveolar capillary endothelium (autoimmune injury).
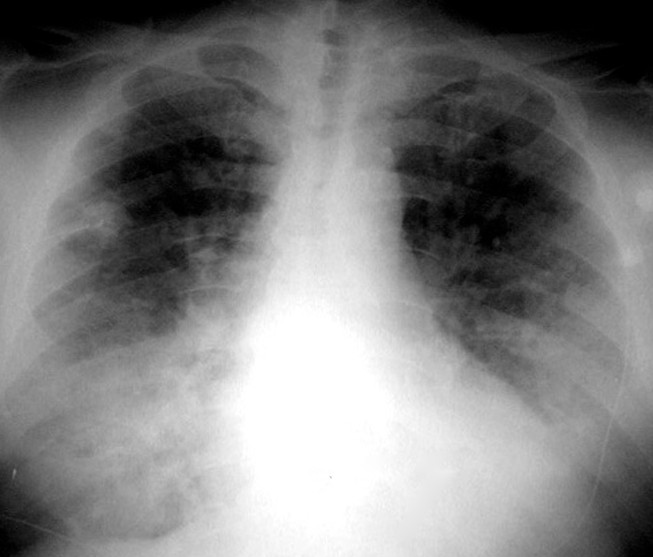
Picture of Diffuse Pulmonary Hemorrhage
Patients who suffer from this form of pulmonary hemorrhage generally present difficulties breathing, with associated hemoptysis and iron deficiency anemia. Other symptoms include: coughing and fever. If acute respiratory failure occurs, there is a high risk of death (emergency treatment is required, with respiratory support). The children who suffer from idiopathic pulmonary hemosiderosis suffer from iron deficiency anemia, with failure to thrive.
The diffuse pulmonary hemorrhage is found in association with the following medical conditions: metastatic lung disease (rare association; the metastases are widespread), coagulative disorders (the pulmonary hemorrhage appears after a precipitating factor, such as infection), Goodpasture syndrome, ATRA syndrome (all-trans-retinoic acid), post bone marrow transplantation, small vessel vasculitis (Wegener granulomatosis, other disorders of the connective tissue, such as systemic lupus erythematosus).
These are the most common methods used for the diagnosis of the diffuse pulmonary hemorrhage:
- Clinical examination of the patient
- Laboratory testing
- CBC – anemia signs
- Imaging studies
- X-ray – bilateral air-space consolidation (relative apical sparing)
- CT chest/HRCT
- Areas of widespread ground glass opacification
- Crazy paving pattern
- Areas of consolidation
- Subacute phase – fine diffuse nodular densities (HRCT)
- Later stage – interlobular septal thickening (intralymphatic accumulation of hemosiderin).
Based on the changes identified on X-rays and CT scans, in the acute phase of the diffuse pulmonary hemorrhage, the differential diagnosis can be made with: multiple localized pulmonary hemorrhage (diffuse aspiration of blood), pulmonary edema and diffuse pulmonary infection (diffuse pneumonia). On the other hand, based on the changes identified on the HRCT, in the sub-acute phase, the differential diagnosis can be made with hypersensitivity pneumonitis.
The treatment of the diffuse pulmonary hemorrhage includes immunosuppressants (for those who suffer from different autoimmune conditions) and respiratory support (in more severe cases, if necessary).
Localized Pulmonary Hemorrhage
The localized pulmonary hemorrhage is a form of hemorrhage that occurs in a particular focal region of the lungs. The extensiveness of the hemorrhage can vary – it can range from a small focus to the complete involvement of a pulmonary lobe.
These are the most common causes that can lead to the appearance of the localized pulmonary hemorrhage: pulmonary vasculitis (granulomatosis with polyangiitis, microscopic polyangiitis), secondary aspiration of blood (chronic bronchitis, bronchiectasis, tumor, infection), pulmonary infarction, tuberculosis, pulmonary vascular tumor infection, trauma (pulmonary contusion, pulmonary laceration), pulmonary arteriovenous malformation, thoracic biopsy (iatrogenic).
The following methods are used for the diagnosis of the localized pulmonary hemorrhage:
- Clinical examination of the patient
- Laboratory testing
- CBC – anemia signs
- Imaging studies
- Chest CT/HRCT scan
- Hazy consolidation or ground-glass infiltration into the parenchyma of the lungs (intraalveolar hemorrhage)
- Peripheral area of ground-glass infiltration (sign of pulmonary vascular tumor invasion – primary neoplasm or metastases).
- Chest CT/HRCT scan
Treatment
These are the most common methods of treatment for the pulmonary hemorrhage:
- Tracheal suction
- Emergency administration of oxygen
- Positive pressure ventilation
- Correction of underlying abnormalities (for example, in the situation that the patient suffers from coagulation disorders)
- Blood transfusion (compensate for the amount of blood that has been lost because of the hemorrhage, prevent future vascular shock).


